Overview of Selected Robotic Prostatectomy Publications
New Surgical Techniques Invented For Robotic Prostatectomy
New Scientific Findings In Robotic Prostatectomy
Educational Book Chapters In Robotic Prostatectomy
Scholarly Review Of Robotic Surgery For Physicians
The University of California, Irvine robotic-assisted laparoscopic prostatectomy experience since its inception in 2002 is one of the oldest programs in the world. UC, Irvine is a leader committed to presenting accurate reproducible techniques and results to expand the potential of robotic prostatectomy and to give the patient accurate information to base their important treatment decisions. UC, Irvine has published the 2nd largest series on robotic prostatectomy in the literature. Since 2003, Dr. Ahlering has written 50+ publications specifically on this new laparoscopic method, of which 7 papers bring forth new advancements in techniques. With nearly 1,000 cases to date, his work demonstrates that robotic prostatectomy produces superior outcomes for the patient in reduced blood loss, nearly zero blood transfusion, low complication rates, earlier return to work, and excellent cancer control outcomes with low positive margin rates. 4,8 The resulting papers, validate the wisdom of the transition from open surgery to the robotic interface.
Additionally, beginning in 2006, we expanded the first results of our new technique for cautery free neurovascular bundle preservation, where ~40% of pre-potent men <66 yrs with unilateral or bilateral nerve preservation return to satisfactory erections within 3 months. 14,15 Perseverance of the surgeon to improve technical methods, and assembly of an excellent surgical team are important standards that UC, Irvine employs. We view validated methods of measuring patient follow-up as essential tools in the assessment and reporting of surgical outcomes.
New Surgical Techniques Invented For Robotic Prostatectomy1. vanVelthoven R., Ahlering TE, Skarecky DW and Clayman RC. Technique for Laparoscopic Running Urethrovesical Anastomosis: ‘The Single Knot Technique’ Urology 61(4):699-702, 2003. 
Summary: One of the initial reasons laparascopic prostectomy was abandoned by its pioneers (Dr. Clayman), was the final step of reconnecting the urethra to the bladder, as one of the final steps of the long, difficult and counterintuitive (reverse) surgery. Many sutures had to be correctly stitched by the reverse laparoscopic technique to prevent the bladder from leaking.
Dr Roland van Velthoven of Belgium had utilized a single ‘running’ stitch, which greatly simplified this technique. Dr. Ahlering proved this clever idea for robotic prostatectomy, and the two published their results jointly. This method has now been adopted as the standard method in robotic and laparoscopic protatectomy, and renamed by many institutions.
2. Lee DI, Eichel L, Skarecky D. Ahlering TE. Robotic Assisted Laparoscopic Radical Prostatectomy with a Single Assistant. Urology 63(6) June 2004.
Summary: Dr. Ahlering has had the privilege of working with excellent urologic fellows who assist his robotic surgery. Working closely as a team, it became rapidly clear that the assistant was more than a passive helper, but could aide the surgeon by correctly positioning the prostate and seminal vesicles to make a safer cleaner dissection. This paper is the first publication to specifically define parts of the surgery where the assistant becomes the 2nd surgeon, and presents that only a single assistant is necessary for the surgery. Additionally this paper documents how to set up the operating theater for accessibility of the surgical instruments and comfort for the assistant.
3. Pick D, Lee DI, Skarecky D, and Ahlering TE. Anatomic Port Placement for the Robotic Prostatectomy. J EndoUrology 18(6):572-575, 2004.
Summary: Because the Robotic instruments are a fixed length (25 cm), they were not able to reach the deepest points of the prostate in the tallest men when using the navel as the landmark.
While not dangerous, it necessitates adding extra ports (holes) in the patient, and adding more time to the surgery. We used the Pythagorem Theorem of triangulation, and identified the pubis as the landmark site, and eliminated this problem. This method is now in common use for robotic prostatectomy.
4. Ahlering TE, Eichel L, Edwards R, Lee DI, Skarecky D. Robotic Radical Prostatectomy: A Technique to reduce pT2 Margins. (+video) Urology 64(6):1224-1228, 2004.
Summary: In men where the cancer is confined to within the prostate, the surgeon may inadvertently nick the prostate and expose the cancer. This is called a PT2 positive margin. This is more likely in open surgery where visibility is more difficult. Dr. Ahlering reviewed his early experience with robotic prostatectomy, and utilizing the high magnification (10-12X) and 3-D color visibility of the da Vinci robotic, refined the technique of prevention of these positive cancer margins. This work produced a surgical technique producing one of the lowest rates reported in the literature, near 5%. This paper is presented with a 7-minute on-line video from the journal showing the technique.
5. Eichel L, Chou D, Skarecky DW, Ahlering TE: Feasibility Study for Laparoscopic Radical Prostatectomy Cautery Free Neurovascular Bundle Preservation. (+video) Urology 65(5):994-997, 2005.
Summary: In a study of dogs, the Walsh group at John Hopkins, identified the damaging effects of electrocautery on the nerves important for the recovery of potency after surgery. 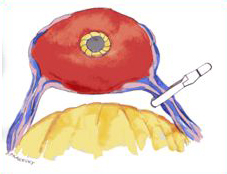
Simultaneously Dr. Ahlering presented a new technique preserving sexual function for robotic prostatectomy by the elimination of the use of electrocautery when preserving the potency nerves of the neurovascular bundle. This technique shows how to carefully control bleeding from the many blood vessels which are intertwined with the potency nerves without the use of damaging electrocautery with a surgery safe clamp (see picture). Without this control, the bleeding obscures the potency nerves, and makes saving these nerves more difficult. This Athermal potency technique has been subsequently adapted as the worldwide robotic surgical standard.
6- Borin J, Skarecky DW, Narula N, Ahlering TE: The Impact of Urethral Stump Length on Continence and Positive Surgical Margins in Robot-assisted Laparoscopic Protstatectomy Urology 70(1): 173-177, 2007.
This new method significantly cut in ½ the overall margin rate of Method I (above) from 17.6 to 7.5%; one of the lowest ever reported. 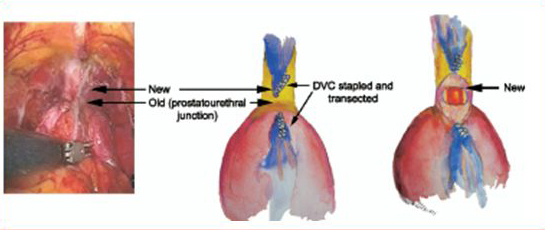
The rate of high-risk pT3 margins were reduced by 4-fold from 50% to 13%. This paper showed these great improvements could be made without impairment to the patient’s continence.
7- Finley DS, Deane L, Rodriquez E, Vallone J, Deshmukh S, Skarecky D, Carpenter P, Narula N, Ornstein DK, Ahlering TE: Anatomic excision of anterior prostatic fat at radical prostatectomy: Implications for pathologic upstaging. Urology 70(5): 1000-1003, 2007.
Summary: A new comprehensive surgical dissection by UCI of the residing fat on and near the prostate eliminates previously undetected cancer positive lymph nodes, which are usually left in robotic prostatectomy. These lymph nodes are present in about 10% of men and 2-4% are positive for prostate cancer.
8- Finley D, Osann K, Skarecky DW, Ahlering TE, Hypothermic nerve sparing radical prostatectomy: rationale, feasibility, and impact of early continence. Urology 73(4) 691-696, 2009. 
Summary: Drs. Ahlering and Finley have taken well established lessons from cardiac and neurosurgeons in using cooling to stop the inflammatory cascade common to all surgical procedures. Think of it as icing one’s ankle immediately upon severely spraining. Actually, we can preemptively cool the region before the injury occurs. Hence, HYPOTHERMIC robotic prostatectomy. We devised an endorectal cooling balloon, pictured left, to locally cool the pelvic region to 60-68oF. The cooling balloon is placed and removed while the patients are asleep. It is safe, easy, painless and remarkably simple. Results on urinary continence demonstrated a reduction from 60 to 40 days to be free of urinary pads. These promising initial results validate the wisdom of preemptive cooling to satisfy the Hippocratic ‘Do no harm’. The impact on sexual function is also a high priority and is actively being studied for improvement.
New Scientific Findings In Robotic Prostatectomy
Cancer Elimination and Control Return of Sexual Function (Potency) after robotic surgery
Return of Urinary control (Continence)
Avoiding complications
Hernia repair during robotic prostatectomy/Avoiding surgical Hernias
Training in Robotic Surgery
Odds and Ends
8. Perer E, Ahlering TE, Lee D and Clayman RC. Robotic Revelation: Laparoscopic Radical Prostatectomy by a non-laparoscopic surgeon. J. Am. Coll. Surgeons, 197(4):693-696, 2003.
Summary: This is the first published report that demonstrates a highly qualified open surgeon can master the robotic technique without transitioning through learning the counterintuitive (reverse) method of straight laparoscopic technique.
9. Ahlering TE, Skarecky DW, Lee DI, and Clayman RC. Successful Transfer of Open Surgical Skills to a Laparoscopic Environment using a Robotic Interface: Initial Experience with the Laparoscopic Radical Prostatectomy. J. Urology 170(5):1738-1741, 2003.
Summary: This study demonstrates a highly qualified open surgeon can master the robotic technique. This initial study demonstrated that the learning curve for robotic prostatectomy was only 15-20 patients versus 40-80 for the straight laparoscopic technique. This study also demonstrated very low blood loss (less than 150cc- about 4 oz of fluid), and complication rate. The time to master the individual steps of the surgery was also presented.
10. Ahlering TE, Woo D., Eichel L, Lee DI, Edwards R, Skarecky D. Robot-Assisted vs. Open Prostatectomy: A comparison of one surgeon's outcomes. rology 63(5) May 2004.
Summary: This early study reviews the safety of the robotic technique as compared to the open technique for one individual surgeon, to eliminate methodological differences between multiple surgeons. This paper showed the robotic technique equaled or exceeded favorable outcomes for the patients undergoing open radical prostatectomy.
11. Ahlering TE, Eichel L, Edwards R, Skarecky D. The Impact of Obesity on Clinical Outcomes in Robotic Prostatectomy. Urology 65(4): 740-744, Dec 2005.
Summary: Robotic prostatectomy can be safely preformed on obese men, but they will take more time in surgery, and may take longer to regain continence.
12. Ahlering TE, Eichel L, Skarecky DW: Early Potency with Cautery Free Neurovascular Bundle Preservation Study in Robotic Laparoscopic Radical Prostatectomy J. Endourology 19(6): 715-718, July/Aug 2005.
Summary: We present the first published results for this new technique for electrocautery free neurovascular bundle preservation for return of potency, where ~50% of pre-potent men, less than 66 years old with unilateral or bilateral nerve preservation, return to satisfactory erections within 3 months.
12 Rodriguez, E., Skarecky DW, Ahlering TE, ‘Perfect’ Continence Outcomes after Laparoscopic Radical Prostatectomy. Urology 67(4): 785-788, 2006.
Summary: In this paper we demonstrated that although obstructive symptoms caused by the prostate will be relieved by robotic surgery, pre existing irritative bladder symptoms will persist after surgery. This work lays the foundation that medications which treat overactive bladders may help men return to continence sooner.
13 Ahlering TE, Borin J, Skarecky DW: Early Potency with Cautery Free Neurovascular Bundle Preservation Study in Robotic Laparoscopic Radical Prostatectomy J. Endourology 20(8): 586-589, July/Aug 2006.
Summary: In this invited paper by the journal, we verified our earlier report of the previous year with approximately twice the number of men. The promising early results remained essentially unchanged bundle preservation for return of potency, where ~45% of pre-potent men, less than 66 years old with unilateral or bilateral nerve preservation, return to satisfactory erections within 3 months.
41. Yee DS, Ahlering TE, Gelman J, Skarecky DW: Fossa Navicularis Strictures in 22F Catheters used in Robotic Radical Prostatectomy. JSLS 11(3), 321-5, 2007.
Summary: Fossa Navicularis Strictures are a complication of surgery that closed down the opening at the tip of the penis, restricting urination. Surprisingly these strictures are caused by using thicker catheters, which were thought to protect the urethra from injury. We showed that using smaller size catheters eliminates this complication.
42. Rodriguez, E., Gill IS, Ahlering TE: Vascular Pedicle Control during Robot-assisted Laparoscopic Prostatectomy: Bulldog Clamp and Suturing Technique. J. Endourology, 22(9):1969-70; 2008
43. Yee DS, Gelman J, Skarecky DW, Ahlering TE: Fossa Navicularis Strictures in Robotic Radical Prostatectomy. J Robotic Surg 1(2):151-154, 2007.
44. Finley DS, Rodriguez, E., Ahlering TE: Combined Inguinal Hernia Repair with Prosthetic Mesh during Transperitoneal Robot-Assisted Laparoscopic Radical Prostatectomy: A Four Year Experience. J. Urology 178:1296-1300, 2007.
Summary: This paper demonstrates our long term outcomes of repairing pre-existing inguinal hernias using the robot during the standard robotic prostatectomy. This procedure added about 15-30 minutes of surgery time. We showed that the robot was very effective at this repair with good long term results.
45. Khan F, Rodriguez E, Finley D, Skarecky DW, Ahlering TE: Implications of Spread of Electrocautery Heat Energy and ‘Heat Sinks’ for Athermal Nerve Sparing Robotic Prostatectomy. J. Endourology, 21(10):1195-1198, 2007
Summary: This paper demonstrates how electocautery causes damage by the transference of heat across urological tissue, and implies how the nerves for sexual function can be heat damage with ensuing loss of sexual function.
46. Ukimura O, Ahlering TE, Gill IG: Transrectal Ultrasound Guided Energy-Free Nerve Sparing Laparoscopic Radical Prostatectomy. J Endourology Sep;22(9):1993-5. 2008
47. Rodriquez E, Skarecky D, Narula N, Ahlering TE: Prostate volume estimation using the ellipsoid formula consistently underestimates actual gland size. J Urology 179(2):501-503, 2008
48. Finley DS, Savatta D, Kopelan A, Ahlering TE: Transperitoneal Robot-Assisted Laparoscopic Radical Prostatectomy and Inguinal Herniorrhaphy. In Press J Robotic Surg.
49. Ahlering TE, Eichel L, Skarecky DW: Evaluation of Long-Term Thermal Injury using cautery during Nerve Sparing Robotic Prostatectomy Urology 72(6):1371-4, 2008.
Summary: This study reviewed the rate of potency return for men who had electrocautery during robotic surgery prior to the new Athermal techniques we introduced. At 2 years potent men ≤ 65 years old had a 63% rate of return of sexual function. A reasonable result but below the new practiced method of Athermal technique.
50. Ahlering TE, Rodriguez E, Skarecky DW, Overcoming Obstacles: Nerve Sparing issues in Robotic-assisted Laparascopic Prostatectomy. J. Endourology 22(4), April 2008.
Summary: This intriguing paper discusses what we have learned about several of the major factors which can impact the return of sexual function after surgery: electrocautery vs Athermal techniques, larger prostate sizes, unilateral vs bilateral nerve sparing. Essentially a result of our dedicated research program to understand sexual function.
51. Ahlering TE, Kaplan A, Yee DS, Skarecky DW. Prostate Weight and Early Potency in Robot-Assisted Radical Prostatectomy Urology 72(6):1263-8, 2008.
Summary: This paper identifies another surgical factor that will impact return of sexual function. We demonstrated that men with larger size prostates (>45 grams) will have a delay in early return to potency at 3 months, probably to traction injury of pulling on a larger prostate during the procedure.
52. Rodriguez E, Finley D, Skarecky DW, Ahlering TE: Single Institution 2 Year Patient-Reported Validated Sexual Function Outcomes after Robotic-assisted Radical Prostatectomy. J Urology 181(1):259-63, 2009.
Summary: This study reviewed the rate of potency return for men who had Athermal nerve sparing during robotic surgery, that we introduced. At 2 years potent men ≤ 65 years old had a 90% rate of return of sexual function, as defined by a yes to both erections and satisfaction. This validated the long term outcomes of our Athermal ( cautery-free) technique.
53. Lavery HJ, Thaly R, Smith JA, Albala D, Ahlering T, Shalhav A, Lee D, Fagin R, Wiklund P, Dasgupta P, Costello AJ, Coughlin G, Patel VR: Robotic Equipment Malfuncation during robotic prostatectomy: a multi-institutional study" J. Endourology 22(9):2165-8, 2008
54. Finley D, Rodriquez E, Skarecky DW, Ahlering TE, Quantitative and Qualitative Analysis of Potency Recovery following Unilateral Nerve sparing Prostatectomy (RLP). BJU Int 104 (10), 1484-1489, Nov 2009.
Summary: Our results support a crossover mechanism for the sexual potency nerves, as men with only one nerve bundle preserved regain sexual function almost as well as those with both nerve bundles preserved. This is an important finding for men who have positive needle biopsies on one side of the prostate, and the cancer threatens to penetrate the prostate into the nerve bundle. If the nerve bundle must be sacrificed to excise the cancer, then the cost to sexual function is not ½ of sexual function but only 10-20%.
55. Gamboa AJ, Santos RT, Sargent ER, Louie MK, Box GN, Sohn KH, Truong H, Lin R, Khosravi A, Santos R, Ornstein DK, Ahlering TE, Tyson DR, Clayman RV, McDougall EM, Long term impact of a Robot Assisted laparoscopic prostatectomy Mini Fellowship Training Program on postgraduate urologica practice patterns. J Urology 181(2): 778-782, 2009.
56. Yee D, Narula N, Amin M, Skarecky DW, Ahlering TE, Robotic-Assisted Laparoscopic Radical Prostatectomy: Current evaluation of surgical margins in clinically low, intermediate, and high risk prostate cancer. J Endourology 23 (9), 1461-1465, Sept 2009.
Summary: This study presents shows that excellent cancer control- i.e. removing all the cancer, can be done with robotic surgery even though the surgeon cannot directly ‘feel’ the prostate. Only a small number of prostate cancers can be ‘felt’, and the paper shows that excellent review of patient’s rectal exam, and pathology features can predict men with high risk of cancer penetrating the prostate.
57. Finley D, Osann K, Chang A, Santos, R, Skarecky DW, Ahlering TE , Hypothermic Radical Prostatectomy: Impact on Continence J Endourology 23 (9), 1443-1450, 2009.
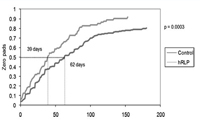 Summary: This study is the first of its kind to explore the use of hypothermia (cooling the rectal area) during radical prostatectomy. This pilot study shows that hypothermia significantly gives an earlier return to pad free urinary continence post surgery.
Summary: This study is the first of its kind to explore the use of hypothermia (cooling the rectal area) during radical prostatectomy. This pilot study shows that hypothermia significantly gives an earlier return to pad free urinary continence post surgery.
58. Zorn KC, Gautam G, Shalhav AL, Clayman RV, Ahlering TE, Albala DM, Lee DI, Sundaram CP, Matin SF, Castle EP, Winfield HN, Gettman MT, Lee BR, Thomas R, Patel VR, Leveillee RJ, Wong C, Badlani GH, Rha KH, Eggener SE, Wiklund P, Mottrie A, Atug F, Kural AR, Joseph JV; Members of the Society of Urologic Robotic Surgeons. Training, Credentialing, Proctoring, Medicolegal Risks of Robotic Urology Surgery: Recommendations of the Society of Urologic Robotic Surgeons, J Urology 182(3): 1126-1132, 2009
59. Lavery HJ, Samadi DB, Thaly R, Albala D, Ahlering T, Shalhav A, Wiklund P, Tewari A, Fagin R, Costello AJ, Coughlin G, Patel VR: The advanced learning curve in robotic prostatectomy: a multi-institutional survey" J. Robotic Surg 3:165-169, 2009.
60. Box G, Kaplan A, Rodriguez E, Skarecky DW, Osann K, Finley D, Ahlering TE,Sacrifice of Accessory Pudendal Arteries in normally potent men during Robotic Assisted Radical Prostatectomy does not impact potency. J Sex Med 7(1): 298-303 Jan 2010.
Summary: It was thought that the Pudendal artery was necessary for preserving sexual function in radical prostectomy by saving this artery’s delivery of blood. We found that sexual function is not dependent on this artery for men did well either with or without it.
61. Liss MA, Canvasser N, Chu W, Chang A, Gan J, Li R, Santos R, Skarecky D, Ahlering TE, Negative impact on Urinary Quality of Life based on Security or 1 Pad versus 0 pads status following Radical Prostatectomy-An evaluation of patient-reported validated questionnaires. J Urology 183(4): April 2010 In press.
Summary: This paper highlights that urinary continence post surgery should be defined as ‘Pad Free’, as men wearing security, one, two or more pads more resemble each other in urinary bother and reported drippage than men pad free. Men should realize that physicians use different definitions of continence, and they should ask what the rate of ‘pad free’ continence is from prospective surgeons.
Educational Book Chapters In Robotic Prostatectomy
Eichel L, Ahlering TE, Clayman, RV. Role of Robotics in Laparoscopic Urologic Surgery. Urologic Clinics of North America. 31(4):781-792, 2004.
Eichel L, Ahlering TE, Clayman, RV. AUA Update Series: Pros and Cons of Robotics in Urological Surgery. AUA Updates 2005.
Borin J, Skarecky DW, Ahlering TE, Robotic Radical Prostatectomy-Onclological Outcomes. In Robotics in Urology Surgery, J. Smith, A. Tewari, Eds, Elsevier Inc. Philadelphia, PA.
Matsunaga G, Costello AJ, Skarecky DW, Ahlering TE Establishment of a Robotic Radical Prostatectomy Program. In Robotic Urologic Surgery, V. Patel, Ed., Springer-Verlag London Ltd, 2007
Basillotte J, Ahlering TE, Skarecky DW. Advances in Surgical Intervention of Prostate Cancer: Comparison of the Benefits and Pitfalls of Retropubic, Perineal and Laparoscopic Radical Prostatectomy. In Prostate Cancer: Signaling Networks, Genetics and New Treatment Strategies. R. Pestell and M. Nevalainen, Eds., Humana Press, Totowa, NJ.
Eichel L, Skarecky DW, Costello AJ, Ahlering TE Nerve Sparing Robotic Prostatectomy Chp 107, In Smith’s Textbook of Endourology, 2nd Ed., G. Preminger, Ed., 2007.
Rodriguez E, Skarecky DW, Ahlering TEOutcome Measures after Robotic-assisted Radical Prostatectomy. In Robotic Urology, H. John and P Wiklund, Eds., Springer, Heidelberg, Germany 2008
Eichel L, and Ahlering TE: Chp 33: Robotics In Urology. In Robotic Surgery. Ed. F. Gharagozloo and F. Najam McGraw Hill Medical., New York NY, 2009.
Goldenberg SL, Ahlering TE, Buchan NC, Skarecky DW, Transitioning from Open to Robotic Radical Prostatectomy-A look back, Chapter 13, In Robotic Urologic Surgery 2nd Ed, V. Patel, Ed., Springer-Verlag London Ltd In Press
Scholarly Review Of Robotic Sugery For Physicians
Ahlering TE.Viewpoint: Robotic versus Laparoscopic Radical Prostatectomy. Nature Clinical Practice-Urology 1(2): 58-59, 2004.
Summary: The Nature journal series is considered to be one of the premier publishers of scholarly material. This article highlights the advantages of robotic prostatectomy over open radical prostatectomy in lower blood loss, lower complication rates, near zero transfusion rates, excellent return to continence, and low margin rates of positive cancer.
Basillotte J., Ahlering TE, Skarecky DW, Lee DI and Clayman RV. Laparoscopic Radical Prostatectomy: Review and Assessment of an Emerging Technique. Surgical Endoscopy 18(12): 1694-1711, July/Aug 2004.
Summary: This is an excellent comprehensive review comparing the three methods of radical prostatectomy: 1. open, 2. laparoscopic, 3. robotic laparoscopic.
Ahlering TE: Editorial Comment - Transperitoneal Laparoscopic Radical Prostatectomy: Ascending Technique. J. Endourology 18(7):599-600, 2004.
Ahlering TE: Editorial Comment - Vattikuti Institute Prostatectomy: A Technique of Robotic Radical Prostatectomy: Experience in more than 1,000 Cases. J. Endourology 18(7):619, 2004.
Ahlering TE, Robotic Prostatectomy is it the Future? Seminar Urologic Urology In Press. 2005
Matsunaga G, Ahlering TE, Skarecky DW. Update on Robotic Laparoscopic Radical Prostatectomy The Scientific World Urology 1, 14-24. DOI 10.1100/tswurol.2006.45
Pick D, Ahlering TE, Omental Splenosis Discovered During Robotic Prostatectomy J Endourol 2008 Aug;22(8):1743-4
Box GN, Ahlering TE, Robotic radical prostatectomy: Long-term outcomes. Curr Op in Urology 18(2):173-179, 2008.
Skarecky DW, Brenner M, Rajan SS, Rodriguez E, Narula N, Melgoza F, Ahlering TE: Zero Surgical Margins after Radical Prostatectomy: Is the end in sight? Expert Rev Med Devices 5(6):709-17, 2008.
Rodriguez E, Skarecky D, Ahlering TE: Salvage Robot-Assisted Radical Prostatectomy with Pelvic Lymph node dissection after Cryotherapy Failure. J. Robotic Surg 1:89-90, 2007.
Rodriguez E, Skarecky D, Ahlering TE: Oncological Outcomes after Robotic-assisted Radical Prostatectomy. Archivo Espanoles de Urologica, 60(4):421-429, 2007 (in English/Spanish).
Yee D, Narula N, Ramzy I, Boker J, Ahlering TE, Skarecky DW, Ornstein DL: Reduced Annexin II Protein in High Grade Prostatic Intraepithelial Neoplasia and Prostate Cancer Arch Pathol Lab Med 131(6):902-908, 2007.
Rodriguez E, Melamud O, Ahlering TE, Nerve-sparing Techniques in open and Laparascopic Prostatectomy. Expert Rev. Anticancer Ther 8(3), 475-479, 2008.